Dauer-Körpernadelakupunktur in Kombination mit Patienten-kontrollierter intravenöser Analgesie (PCIA) zur Verbesserung der Genesung von Patientinnen nach laparoskopischer Myomektomie: Eine randomisierte, kontrollierte Studie
Abstract
Background
Pain and gastrointestinal dysfunction after laparoscopic myomectomy (LM) are significant issues that prevent this procedure from being classified as a “Day Surgery.” This study aims to assess the effectiveness and safety of thumbtack needle acupuncture (TNA) combined with patient-controlled intravenous analgesia (PCIA) for promoting enhanced recovery after LM.
Methods
A total of 52 patients were enrolled in the study, divided into a treatment group receiving TNA and a control group. Both groups were administered PCIA without background sufentanil. For rescue analgesia or antiemetic needs, a bolus infusion of flurbiprofen axetil (50 mg) or intravenous metoclopramide (10 mg) was provided. The primary outcomes measured were the Visual Analog Scale (VAS) scores at awakening, as well as at 36 h, 48 h, and 60 h after LM. Secondary outcomes included VAS scores at 6 h, 12 h, 24 h, and 72 h after LM, total sufentanil consumption, the number of PCIA analgesic requests (attempts), the number of doses of rescue flurbiprofen axel analgesia required, preoperative anxiety scores, gastrointestinal function recovery assessment, first ambulation time, length of hospital stay, and patient satisfaction. Adverse events were also recorded.
Results
Compared to the control group, the treatment group showed significantly lower VAS scores, fewer analgesia attempts, reduced total sufentanil consumption, and a smaller number of rescue analgesia doses after LM, along with lower preoperative anxiety scores and higher satisfaction with pain management (p < 0.05). Gastrointestinal function recovery was enhanced in the treatment group, as indicated by earlier flatus and defecation, a lower incidence of postoperative nausea and vomiting (PONV), and a smaller number of metoclopramide doses required (p < 0.05). Additionally, ambulation occurred earlier, and the length of hospital stay was shorter in the treatment group (p < 0.05). No adverse events were observed in patients receiving TNA.
Conclusion
TNA is a safe intervention that effectively alleviates postoperative pain, decreases the total consumption of sufentanil, reduces preoperative anxiety, enhances the recovery of gastrointestinal function, and shortens the duration of hospitalization, making it an ideal adjunct treatment for postoperative recovery after LM. Further research is required to understand the mechanisms underlying this intervention.
Autoren
Peiyu Mao, Weijie Meng, Tongxin Mao, Hui Li, Xuqun Xu, Xuelu Jiang, Huadi Yang
Journal
Frontiers in Medicine
Link: https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2024.1485211/full
DOI: https://doi.org/10.3389/fmed.2024.1485211
Kommentar:
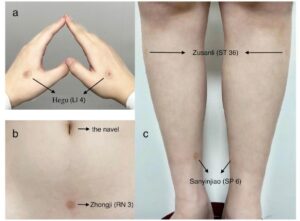
Hier wurden die Punkte mit einer Pyonex Dauerakupunkturnadel stimuliert (siehe Bild)
Verwendete Punkte: Dickdarm 4 (LI4), Milz 6 (SP6), Magen 36 (ST36), Ren Mai 3 (RN3)